You’ve had a PET scan, and now your report mentions something called “FDG uptake” in various parts of your body. The term sounds technical and maybe a bit worrying. Let’s break down what this actually means and why doctors pay close attention to it.
What Exactly Is FDG?
FDG stands for fluorodeoxyglucose—a radioactive form of glucose (sugar). Think of it as a glucose molecule with a tiny radioactive tracer attached to it. Before your PET scan, a technician injects this substance into your vein, usually in your arm.
Your body treats FDG almost exactly like regular sugar. Cells absorb it the same way they absorb glucose from your bloodstream. But there’s one crucial difference: once FDG enters a cell, it gets partially trapped inside. This trapping effect allows the PET scanner to detect where the FDG has accumulated in your body.
The radioactive part emits positrons—tiny particles that the scanner can detect. When these positrons collide with electrons in your body, they produce gamma rays. The PET scanner picks up these gamma rays and creates detailed images showing where the FDG has concentrated.
Why Doctors Use FDG?
Glucose fuels nearly everything your body does. Your cells need it for energy, growth, and repair. But different cells consume glucose at different rates. Active cells gobble up more glucose than quiet, resting cells.
Cancer cells, for instance, typically metabolize glucose at much higher rates than normal cells. They’re growing rapidly and dividing constantly, which requires tons of energy. This hungry behavior makes them light up on PET scans when they absorb FDG.
But cancer isn’t the only thing that causes high FDG uptake. Your brain uses massive amounts of glucose even when you’re just sitting still. Your heart needs glucose to keep pumping. Muscles that have been working hard will show increased uptake. Even inflammation from infections or injuries increases glucose metabolism in affected areas.
Normal vs Abnormal Uptake Patterns
Brain
Your brain normally shows intense FDG uptake—it’s one of the most metabolically active organs in your body. The gray matter (where most brain cells live) typically shows higher uptake than white matter (mostly nerve fibers). This pattern is completely normal and expected.
Heart
Heart muscle uptake varies depending on what you’ve eaten recently and how your body is using fuel. Sometimes the heart shows strong uptake, other times minimal uptake. Both patterns can be normal. Doctors compare your heart uptake to established patterns to determine if something looks concerning.
Liver and Spleen
These organs show moderate, uniform FDG uptake in healthy people. The liver processes nutrients and filters blood, while the spleen filters old blood cells—both activities require steady energy. Patchy or unusually intense uptake might indicate problems.
Kidneys and Bladder
Your kidneys filter FDG from your blood and excrete it into urine. This means both organs normally show high uptake. The bladder often appears as a bright spot on PET images simply because it’s collecting radioactive urine. This is completely expected and not concerning.
Bone Marrow
Your bone marrow makes new blood cells constantly, which requires energy. Mild FDG uptake in bones, especially the spine, pelvis, and sternum, is normal. The pattern should look relatively symmetric on both sides of your body.
Muscles
Muscles that have been active before your scan will show increased uptake. If you exercised that morning or tensed up during the injection, those muscles might light up. Talking, chewing gum, or even shivering from cold can cause uptake in jaw and neck muscles.
Brown Fat
Some people have brown adipose tissue (brown fat) that activates in cold conditions. This fat burns calories to generate heat, which means it absorbs FDG. It typically appears in the neck, shoulders, and along the spine. It looks concerning at first glance but is actually harmless metabolic activity.
What High Uptake Means
When doctors talk about “increased FDG uptake” or “hypermetabolic activity,” they mean an area is consuming more glucose than surrounding tissues. The uptake gets measured using something called SUV (Standardized Uptake Value)—a number that quantifies how much FDG has accumulated in a specific spot.
SUV values help doctors distinguish between normal and abnormal uptake. Generally:
- SUV below 2.5: Often considered normal or benign
- SUV between 2.5-5: Gray zone that needs clinical context
- SUV above 5: More suspicious for malignancy
But these numbers aren’t absolute rules. A reading of 3 might be worrying in one organ but perfectly normal in another. Context matters tremendously.
Causes of Increased Uptake
Cancer
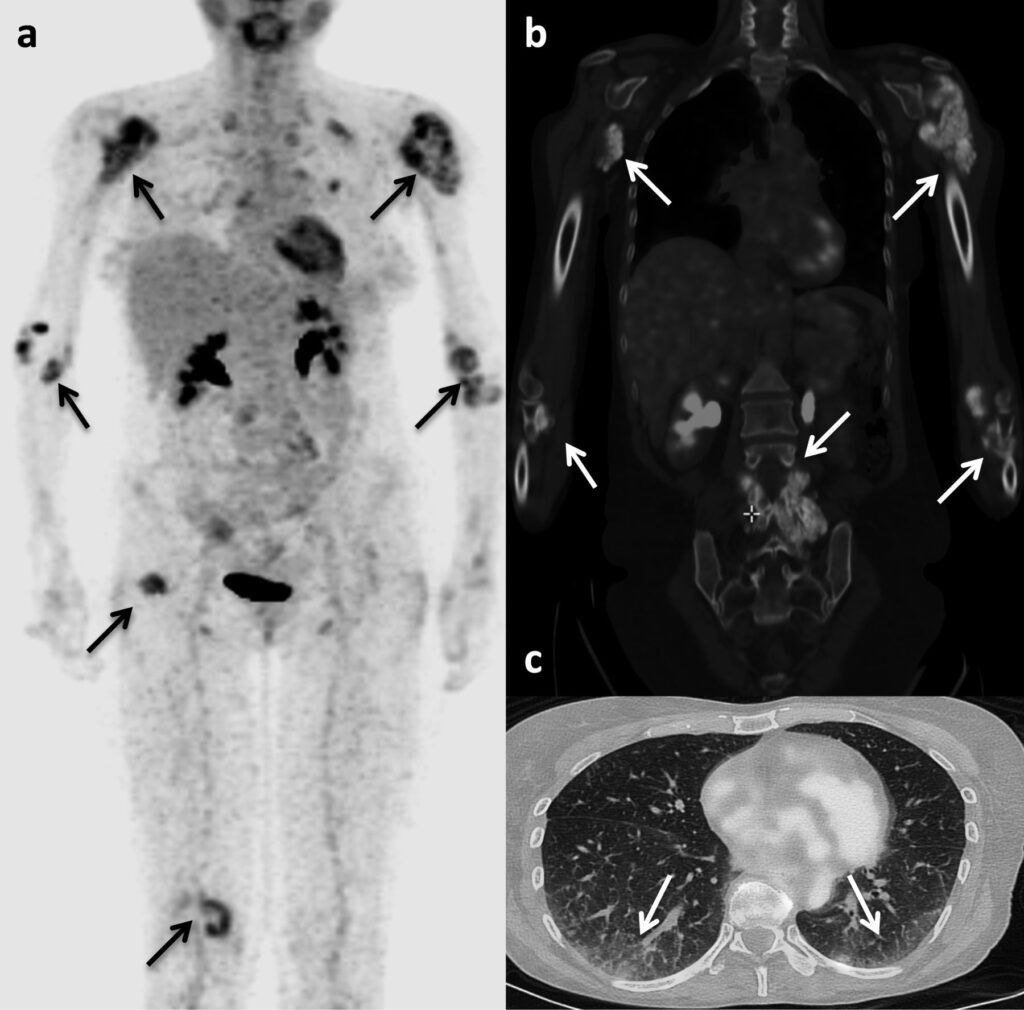
Malignant tumors typically show markedly elevated FDG uptake because cancer cells divide rapidly and need lots of energy. Most (but not all) cancers are “FDG-avid,” meaning they absorb the tracer enthusiastically. This makes PET scans particularly useful for detecting cancer, staging disease, and monitoring treatment response.
However, not all cancers show high uptake. Some slow-growing tumors or certain cancer types (like prostate cancer or some kidney cancers) may show minimal FDG accumulation. A negative PET scan doesn’t always rule out cancer.
Infection and Inflammation
Your immune system cells become metabolically active when fighting infections. White blood cells rush to infection sites, where they consume glucose to fuel their defensive activities. This creates hot spots on PET scans that can look similar to cancer.
Inflammatory conditions—arthritis, sarcoidosis, inflammatory bowel disease—also cause increased uptake. Recent surgeries or injuries show uptake during the healing process. Even vaccine injections can cause temporary uptake in nearby lymph nodes.
Benign Growths
Not all growths are cancerous, but benign tumors might still show FDG uptake if they’re metabolically active. Adenomas (benign glandular tumors), fibroids, and other non-cancerous masses can light up on scans.
Normal Physiological Activity
We’ve touched on this already, but it bears repeating: lots of normal body functions cause FDG uptake. Your gut shows variable uptake depending on digestion. Ovaries show cyclic uptake patterns related to menstrual cycles. Muscles you’ve used recently will show uptake. Stress and anxiety can increase overall metabolism.
Low or Absent Uptake
Sometimes the concern isn’t high uptake but rather lower-than-expected uptake. Dead or dying tissue doesn’t metabolize glucose, so it appears dark on PET images. Scar tissue from old injuries or surgeries shows minimal uptake.

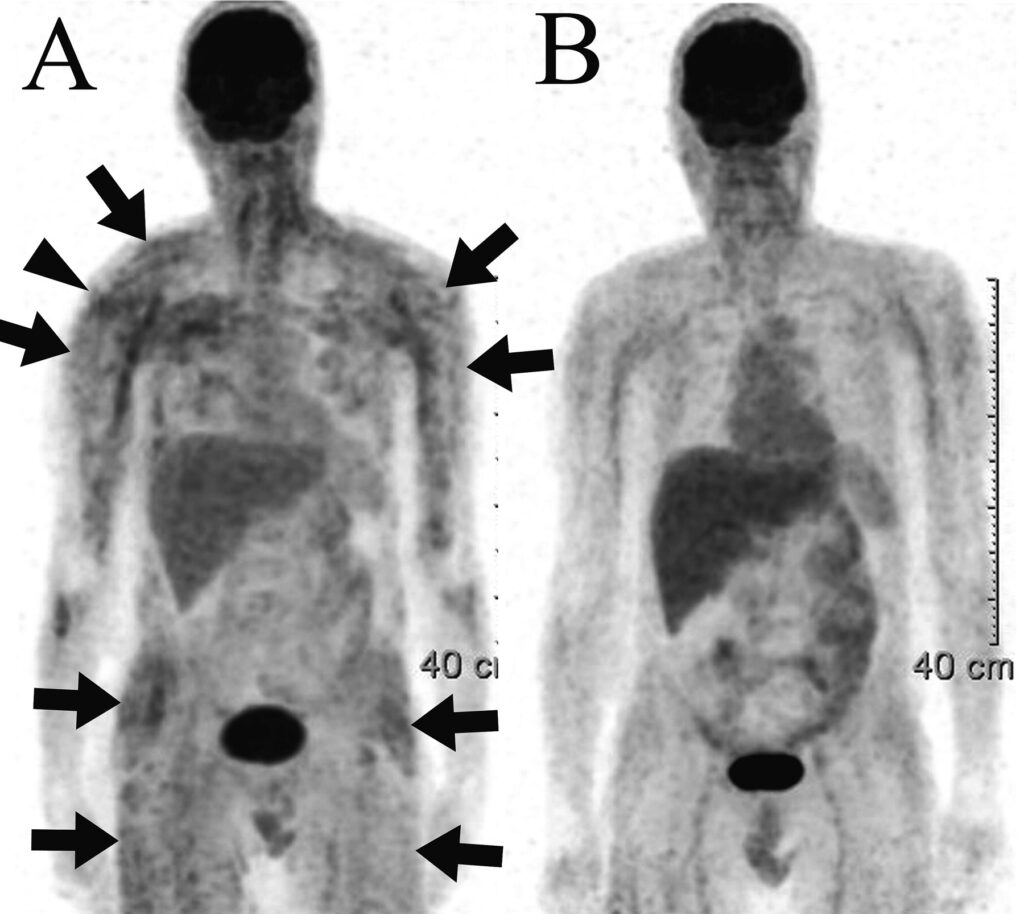
After cancer treatment, doctors want to see decreased uptake in tumor areas—this suggests the treatment is working and cancer cells are dying. Persistent high uptake after therapy might indicate resistant, viable tumor cells.
Some organs or tissues naturally show low uptake. Fatty tissue, for example, has low metabolic activity. Lung tissue (the air sacs, not the blood vessels) shows minimal uptake in healthy people.
Reading Your PET Scan Report
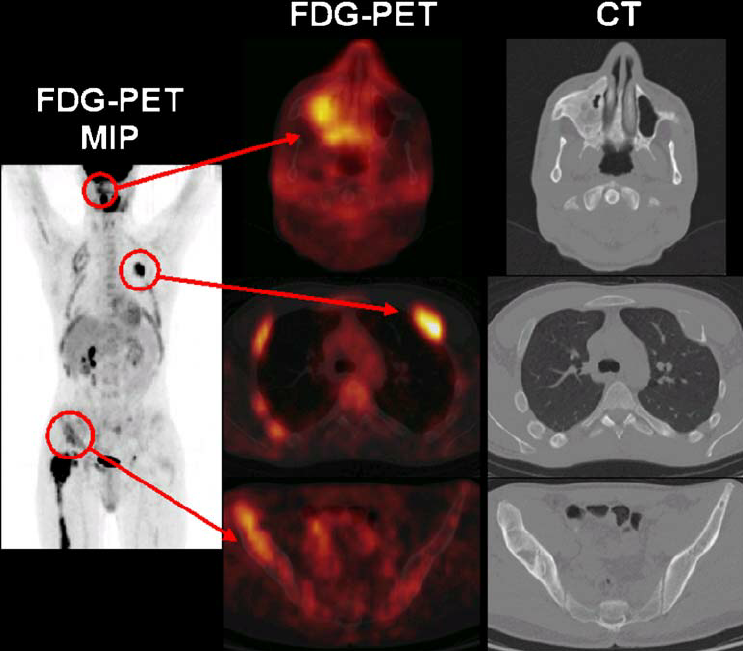
Your report probably mentions uptake in various locations along with SUV numbers. The radiologist describes the pattern, intensity, and location of uptake throughout your body.
“Physiologic uptake” means normal, expected activity. “Pathologic uptake” suggests something abnormal that needs attention. Terms like “focal” (one specific spot), “diffuse” (spread out), “intense,” or “mild” describe the pattern and degree of uptake.
The report might compare your current scan to previous ones, noting whether areas of uptake have increased, decreased, or stayed stable. Changes over time provide crucial information about disease progression or treatment effectiveness.
Limitations and False Positives
PET scans are powerful diagnostic tools, but they’re not perfect. False positives happen—areas that light up but turn out to be benign. As mentioned, infections, inflammation, recent injuries, and normal physiological processes can all mimic concerning uptake patterns.
False negatives occur too. Small tumors (under 5-7mm) might not show up because they haven’t accumulated enough FDG to detect. Certain cancer types naturally show low glucose metabolism. High blood sugar levels can interfere with FDG uptake, making tumors harder to see.
This is why doctors never rely solely on PET scan results. They combine PET findings with CT or MRI images, blood tests, physical exams, and sometimes tissue biopsies to reach accurate diagnoses.
Preparing for Accurate Results
Your preparation before the scan significantly affects uptake patterns. Fasting for 4-6 hours beforehand ensures your blood sugar stays low, which improves FDG uptake into cells. High blood sugar causes cells to prefer regular glucose over FDG, making the scan less sensitive.
Avoiding exercise for 24 hours before the scan prevents muscle uptake that could confuse the images. Staying warm and relaxed minimizes brown fat activation. Some facilities provide warm blankets and keep rooms comfortable to prevent shivering.
Following these preparation instructions helps ensure your scan shows true pathologic uptake rather than artifacts from normal activities.
FAQs
How long does the FDG stay radioactive in my body?
FDG has a half-life of about 110 minutes, meaning every 110 minutes, the radioactivity decreases by half. Within 24 hours, nearly all radioactivity leaves your system through urine. Drinking extra water helps flush it out faster.
Can I be around children or pregnant women after my scan?
Most facilities recommend avoiding close, prolonged contact with young children and pregnant women for 6-12 hours after injection. The radiation exposure is minimal but this precaution reduces any theoretical risk. Brief interactions are generally fine.
Why do I need to fast before a PET scan?
Fasting lowers your blood sugar, which makes cells more eager to absorb the injected FDG. High blood sugar from eating causes cells to use regular glucose instead, reducing FDG uptake and making the scan less effective at detecting abnormalities.
Can diabetes affect my PET scan results?
Yes, elevated blood sugar in diabetic patients can interfere with FDG uptake and reduce scan sensitivity. Your blood sugar level gets checked before injection. If it’s too high, the scan might be rescheduled. Take your diabetes medications as directed unless told otherwise.
What’s the difference between a PET scan and a PET/CT scan?
A PET/CT combines metabolic information from the PET scan with detailed anatomical images from CT. The CT shows structures clearly while the PET shows which areas are metabolically active. Together, they pinpoint exactly where abnormal uptake is occurring.
Does high uptake always mean cancer?
No. Infections, inflammation, recent injuries, healing tissues, and normal physiological processes all cause increased uptake. Doctors consider uptake patterns, SUV values, clinical symptoms, and other tests before making diagnoses. Context is everything.
Can medications affect FDG uptake?
Some medications can influence uptake patterns. Insulin drives glucose (and FDG) into muscles, potentially causing diffuse muscle uptake. Certain chemotherapy drugs, growth factors, and steroids might affect results. Tell your doctor about all medications you’re taking.
How accurate are PET scans for detecting cancer?
PET scans are highly sensitive for most cancers, detecting about 85-95% of metabolically active tumors. Accuracy varies by cancer type—some cancers (lymphoma, lung cancer, melanoma) show up better than others (prostate, kidney). Combining PET with CT improves accuracy.
What if my scan shows uptake but the biopsy is negative?
This happens occasionally. The uptake might represent inflammation, infection, or a benign process that mimics cancer. Sometimes biopsies miss the target or sample non-representative tissue. Your doctor might recommend repeat imaging, additional biopsies, or monitoring over time.
Can I have a PET scan if I’m claustrophobic?
PET scanners are more open than MRI machines. You lie on a table that passes through a large ring—it’s not an enclosed tube. Most claustrophobic patients tolerate PET scans without problems. If you’re very anxious, discuss options with your doctor beforehand.
Why does my report mention different SUV numbers?
Reports often include SUVmax (highest uptake in a region), SUVmean (average uptake), and SUVpeak (average of highest voxels). Each measurement provides slightly different information. SUVmax is most commonly used but can be affected by image noise.
How soon after treatment can I get a follow-up PET scan?
Timing depends on the treatment type. After chemotherapy or radiation, doctors often wait 8-12 weeks before scanning. Inflammation from treatment can cause temporary uptake that might be mistaken for active disease. Too-early scans can give misleading results.
What Happens After Your Scan
The radiologist analyzes your images and writes a detailed report describing all areas of FDG uptake. This report goes to your referring doctor, who interprets the findings in the context of your symptoms, medical history, and other test results.
Your doctor might recommend additional imaging, biopsies of suspicious areas, or simply monitoring over time with follow-up scans. Treatment plans often depend partly on PET scan findings—they help doctors determine cancer stage, select appropriate therapies, and track treatment response.
If your scan shows unexpected uptake, don’t panic. Many things cause increased FDG accumulation, and not all of them are serious. Your doctor will guide you through the next steps based on your specific situation.
More Posts:
