When dealing with unexplained pain, numbness, or weakness, you might wonder if an MRI scan can reveal what’s happening to your nerves. MRI technology has become quite skilled at spotting various types of nerve problems, though it’s not perfect for every situation.
How MRI Spots Nerve Problems?
MRI machines work by creating detailed pictures of soft tissues in your body using magnetic fields and radio waves. Unlike X-rays that mainly show bones, MRI excels at revealing muscles, tendons, and yes – nerves too.
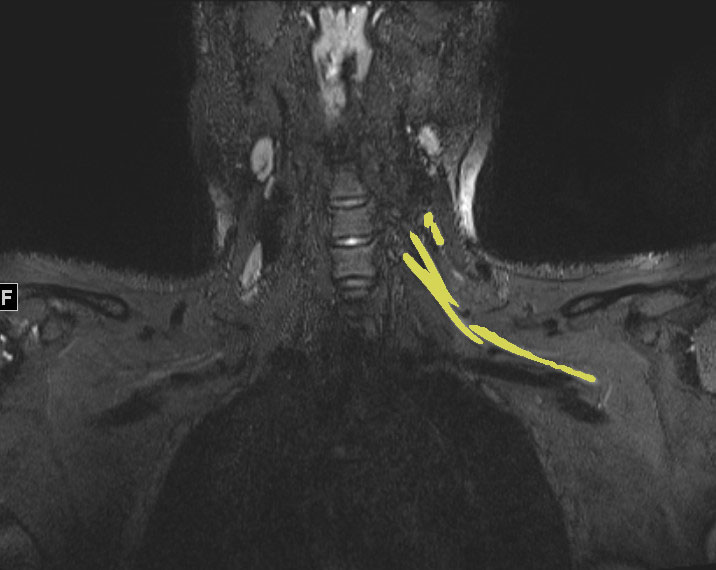
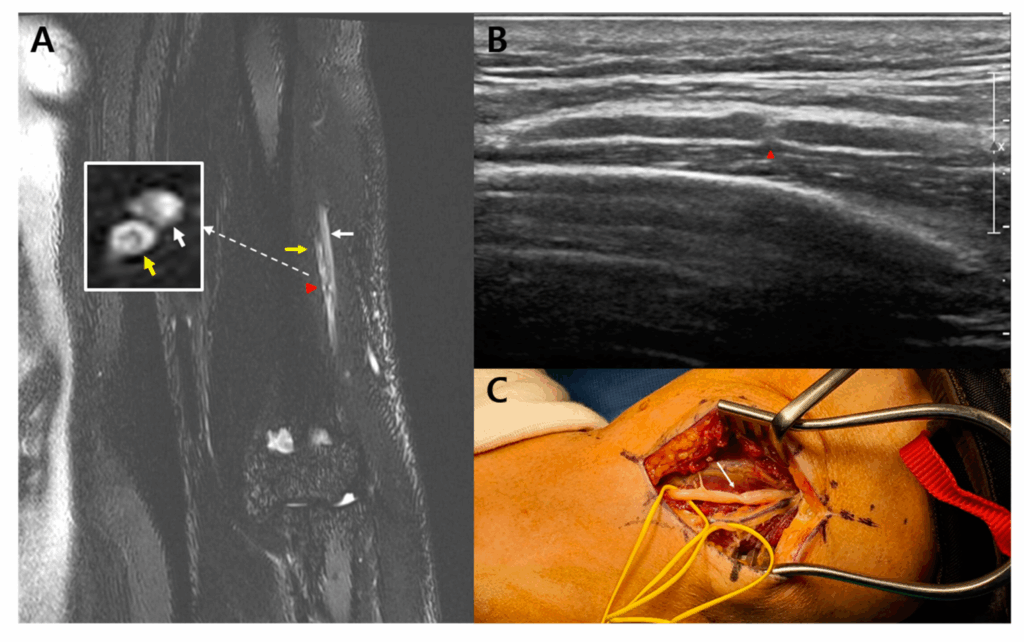
The technology can pick up on several signs that point to nerve damage. Swollen nerves often appear brighter than normal on certain MRI sequences. Compressed nerves may look flattened or show unusual signal changes. Sometimes the scan reveals what’s pressing on a nerve – like a herniated disc pushing against spinal nerve roots.
What Nerve Problems Show Up Best on MRI?
Certain types of nerve damage appear more clearly than others on MRI scans. Larger nerves tend to show up better than tiny ones, simply because there’s more tissue to image.
Spinal nerve issues often appear quite well on MRI. When discs bulge or herniate, they frequently press against nerve roots, creating visible compression. Spinal stenosis – where the spinal canal narrows – also shows up clearly as the space around nerves becomes cramped.
Peripheral nerves in your arms and legs can also be seen on MRI, especially when they’re significantly swollen or compressed. Carpal tunnel syndrome sometimes appears on specialized wrist MRI scans, showing the median nerve getting squeezed in the narrow tunnel at your wrist.
Nerve tumors, though rare, typically show up quite well on MRI scans. These growths create distinct patterns that radiologists can often identify.

When MRI Might Miss Nerve Damage?
Despite its impressive capabilities, MRI has limitations when it comes to nerve problems. Very small nerve fibers may not show up at all, even when they’re damaged. Some types of nerve injury – particularly those affecting function rather than structure – might not create visible changes on the scan.
Early-stage nerve damage sometimes hasn’t progressed enough to create noticeable changes in appearance. The nerve might not be working properly, but it still looks normal on imaging.
Certain conditions affect nerve function without changing how nerves look. Diabetic neuropathy, for instance, typically damages nerves at a microscopic level that MRI can’t detect.
Other Tests That Work Alongside MRI
Doctors often combine MRI with other tests to get a complete picture of nerve health. Electromyography (EMG) and nerve conduction studies measure how well nerves actually function, rather than just how they look. These tests can catch problems that MRI might miss.
Blood tests can reveal underlying conditions that damage nerves, like diabetes or vitamin deficiencies. Clinical examination – testing reflexes, sensation, and strength – provides crucial information about nerve function that imaging alone can’t capture.
What to Expect During the Process?
If your doctor orders an MRI to check for nerve problems, the scan itself is painless but can be lengthy – often 30 to 60 minutes depending on what areas need imaging. You’ll lie still inside a tube-shaped machine that makes loud knocking sounds.
Some nerve-focused MRI scans use special sequences designed to highlight nerve tissue more clearly. These might take longer than standard scans but can provide more detailed information about nerve health.
Contrast dye isn’t always needed for nerve imaging, but sometimes it helps highlight inflammation or other changes around nerves.
Making Sense of Results
MRI results don’t always tell the whole story. A scan might show structural problems that aren’t causing symptoms, or symptoms might exist without visible changes on the scan. This is why doctors consider MRI findings alongside your symptoms and other test results.
The timing of the scan matters too. Very recent nerve injuries might not show changes yet, while very old injuries might have healed enough that damage is no longer visible.
Frequently Asked Questions
How accurate is MRI for detecting nerve damage?
MRI accuracy varies depending on the type and location of nerve damage. It’s quite good at detecting compressed or significantly swollen nerves, with accuracy rates often above 80-90% for these conditions. However, it may miss subtle nerve damage or early-stage problems.
Can MRI see pinched nerves?
Yes, MRI often shows pinched nerves quite well, especially in the spine. The scan can reveal what’s compressing the nerve (like a herniated disc) and show changes in the nerve itself from the compression.
Will nerve damage always show up on MRI?
No, not all nerve damage appears on MRI. Very small nerve fibers, early-stage damage, and functional problems without structural changes may not be visible on the scan.
How long does a nerve MRI take?
Most MRI scans for nerve problems take 30-60 minutes. Specialized nerve imaging sequences might extend this time, but the exact duration depends on which body parts need scanning and what specific information doctors are seeking.
Do I need contrast for a nerve MRI?
Not always. Many nerve problems can be seen without contrast dye. Your doctor might recommend contrast if they suspect inflammation, infection, or tumors affecting nerves.
Can MRI detect old nerve injuries?
Yes, sometimes. Very old nerve injuries might show up as scar tissue or permanent changes in nerve structure. However, if nerves have healed well over time, old injuries might not be visible anymore.
What’s the difference between MRI and nerve conduction studies?
MRI shows the structure and appearance of nerves, while nerve conduction studies test how well nerves actually function. Many doctors use both tests together since they provide different but complementary information about nerve health.
The Bottom Line
MRI can detect many types of nerve damage, particularly when nerves are compressed, swollen, or structurally altered. It works best for larger nerves and problems that create visible changes in nerve appearance or surrounding tissues.
However, MRI isn’t a perfect test for nerve problems. It might miss subtle damage or functional issues that don’t create structural changes. The most effective approach often combines MRI with other tests and careful clinical evaluation.
If you’re dealing with symptoms that might indicate nerve problems, discuss with your doctor which tests would be most helpful for your specific situation. MRI might be part of the answer, but it’s rarely the only piece of the puzzle.
